2026 Dual Special Needs plan (D-SNP) updates
Changes are here for Dual Special Needs plans
The Centers for Medicare & Medicaid Services (CMS) has made changes to the rules for Dual Special Needs plans (D-SNPs). These changes apply to all insurers — not just UnitedHealthcare — and may affect your D-SNP benefits and when you can sign up for or change your plan. We know it can be hard to understand how to get the most from your coverage, especially when things change. You can count on UnitedHealthcare to provide you with reliable Medicare information and support every step of the way.
What’s changing for D-SNP benefits in 2026?
CMS has ended a program called the Value-Based Insurance Design (VBID) model. Here's what this means for you:
End of $0 copayments for prescriptions
With VBID no longer being offered, many Part D plans will no longer be able to offer all covered drugs at $0. Some insurers may still offer savings on prescription drugs through different programs, and members won’t pay more than the copayments (copays) aligned to their level of Extra Help.
New qualifications for supplemental benefits
Eligibility for non-medical supplemental benefits, such as a credit for healthy food and home utilities, will be based on verification of a qualifying chronic condition. Conditions may include chronic high blood pressure, diabetes, cardiovascular disease and more.
For 2026, verification of a qualifying condition will be required to spend your monthly OTC credit on healthy food and utilities. But, there’s good news. We've already verified a qualifying condition for 95% of our eligible members. This verification process is exclusive to UnitedHealthcare. Verified status does not transfer to other Medicare Advantage brands.
Important Dual Special Needs plan changes explained
2026 D-SNP benefit changes: What You Should Know
A nationwide policy change may affect benefits in 2026
- The Centers for Medicare & Medicaid Services has ended the VBID program, which allowed Dual Special Needs plans to offer $0 copays on all covered Part D prescriptions and provide additional benefits like credits to help pay for food and utilities, rides and housing.
- The Extra Help program will help keep prescription costs lower and some additional savings may be available through other programs, depending on your plan.
- For additional benefits like a credit for healthy food and home utilities, you will need to verify a qualifying chronic condition such as chronic high blood pressure, diabetes or cardiovascular disease. Before the Annual Enrollment Period (October 15 to December 7), watch for an Annual Notice of Change (ANOC) from your insurer. This notice will include information about benefits that are affected.
- Before you enroll, we recommend reviewing your plan’s benefits to ensure they meet your health and financial needs. If you need to make a change, you can contact your insurer or speak with a local agent to learn about plans and coverage.
*Plans may not be available in all areas/markets.
What changed for D-SNP enrollment periods in 2025?
Monthly Special Enrollment Period (SEP)
If you're eligible for Medicare and have full Medicaid benefits, there is now a monthly Special Enrollment Period.
Special Enrollment Period limited to integrated plans
During this new Special Enrollment Period, you may enroll in select D-SNPs from the same insurer who manages your Medicaid coverage.
2025 enrollment changes explained

Find the right Medicare plan for all your plans
Enter your ZIP code to see what plans are available in your area.
Here's what you need to know:
Monthly chance to switch between integrated D-SNPs for dual eligibles
- If you’re eligible for Medicare and have full Medicaid benefits, there is a new monthly SEP instead of the quarterly ones you may be used to.
- Integrated care SEPs allow enrollment in select D-SNPs and Medicaid plans under one insurer.
- Beside this new monthly enrollment period, all dual-eligible beneficiaries can still enroll during the Annual Enrollment Period (AEP) or a Medicare Special Enrollment Period with a qualifying life event. There may be other opportunities to enroll as well.
*Plans may not be available in all areas/markets.
New enrollment rules will make Medicare and Medicaid work better together
- Starting in 2025, if you are eligible for Medicare and have full Medicaid benefits, there is a new monthly SEP that may help combine your Medicare and Medicaid coverage with one insurer.
- During this monthly SEP, you may sign up for a D-SNP from the same insurer that manages your Medicaid coverage.
- Qualified plan options for this enrollment period depend on where you live and which insurer you use.
- This Special Enrollment Period does not apply if you have partial Medicaid benefits or just Extra Help, also known as Low-Income Subsidy (LIS).
*Plans may not be available in all areas/markets.
Additional resources and materials
Explore videos and articles for more in-depth information about Dual Special Needs plans.
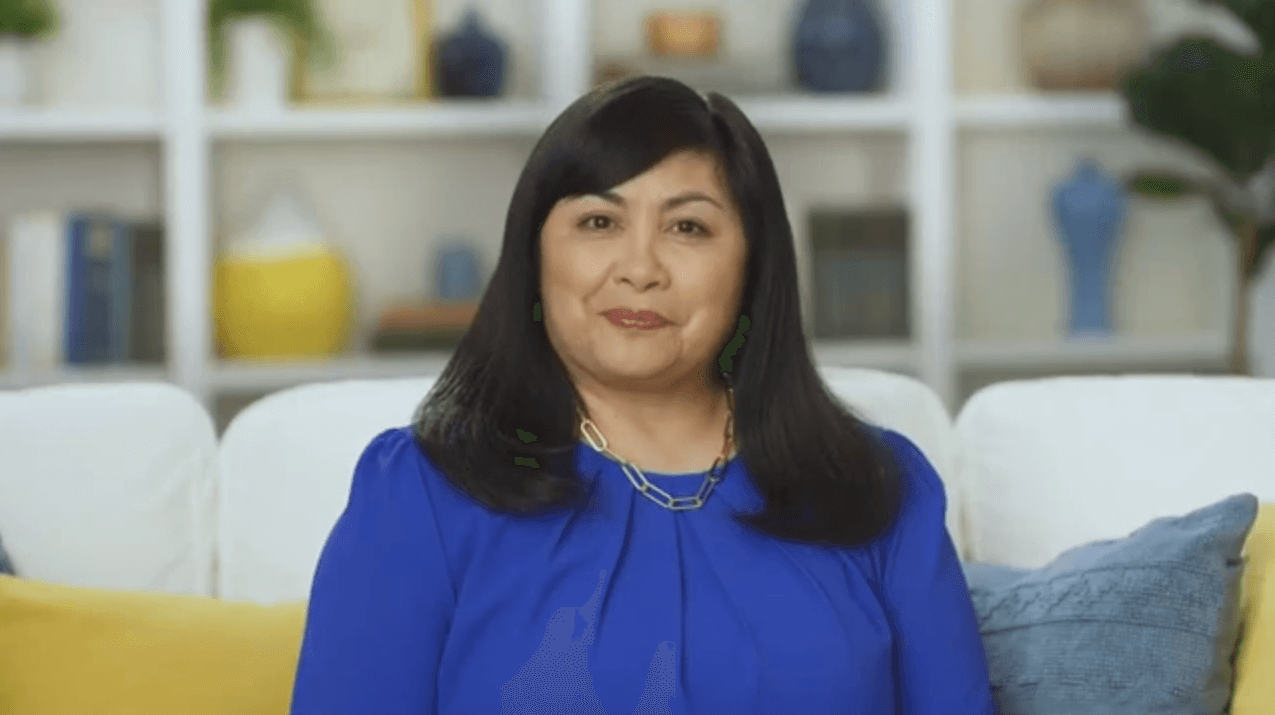
From choosing your plan to using your plan, we're committed to helping you every step of the way.
Find the right Medicare plan for all your plans